Type 2 diabetes mellitus (T2DM) is a significant, growing health problem that results in increased morbidity and mortality. In adults, T2DM accounts for about 90% to 95% of all diagnosed cases of diabetes.1 Diabetes is the leading cause of kidney failure and blindness; moreover, diabetic patients are 2 to 4 times more likely to die of complications of heart disease and/or have a stroke.2 Other complications of diabetes include nervous system damage and nontraumatic lower limb amputation. Increased morbidity and mortality not only diminishes quality of life (QOL) for patients with diabetes, but also produces a financial health care burden. The cost of diabetes in the U.S. in 2012 was more than $245 billion compared with $174 billion in 2007.1
The Centers for Disease Control and Prevention (CDC) predicts that 1 in 3 American adults will develop diabetes by 2050; thus, optimal approaches to diabetic care need to be developed and evaluated to determine best practices.3,4 Better control of blood sugar, cholesterol, and blood pressure levels in people with diabetes will help reduce the risk of complications of kidney disease, eye disease, nervous system disease, heart attack, and stroke.5 Optimal approaches to diabetes management must now be developed to prepare for the forecasted increase of T2DM.
A review of the literature confirms that lack of continuity of care often leads to patient dissatisfaction with health care, to fragmented health care, and a greater propensity to disregard a defined health care treatment plan.6,7 In addition to improved patient satisfaction and adherence to medical management, improved continuity of care is cost-effective. A longitudinal study based on claims data from 2000 to 2008, using the continuity of care index, indicated that improved continuity of care was associated with less health care waste and lower health care expenses for patients with T2DM.8 An average savings of $737 in total health care expenses per person was achieved with better continuity of care.8 These studies demonstrate that improving continuity of care improves outcomes in patients with diabetes and helps prevent excessive health care costs and waste.
Medical Center NonContinuity
Lack of continuity of care has been identified as a potential obstacle to optimal diabetic outcomes at William Beaumont Army Medical Center (WBAMC) in El Paso, Texas, based on a recent data analysis provided by TRICARE Regional Office West.9,10 As of March 2010, 56,936 patients were enrolled in TRICARE Prime. Of these patients, only 29.92% had appointments with their assigned primary care manager (PCM).9
In 2009, WBAMC developed a database to track the Healthcare Effectiveness Data and Information Set (HEDIS) measures to monitor A1c as well as other indicators of performance of health care services, such as mammography, Pap smear, bone densitometry, and colorectal screening. A recent American Diabetic Association expert committee recommendation endorsed the use of A1c value > 6.5% to confirm the diagnosis of diabetes.11 The A1c test may be confirmed with a repeat test unless clinical symptoms exist or the patient has random glucose levels > 200 mg/dL. Importantly, individuals with an A1c between 6% and 6.5% have a higher risk for developing diabetes and may be diagnosed with prediabetes.3
From 2008 to 2009, the HEDIS database tracking the progress of A1c demonstrated a 0.3% positive change and improvement in A1c ≤ 9% (normal 4%-6%). The goal for people with diabetes is A1c < 7%. Uncontrolled diabetes, (ie, A1c > 9%), is associated with greater diabetes-related complications.12 Using the HEDIS benchmark of ≥ 9%, the HEDIS A1c data for fiscal year (FY) 2008 were 71.1 (p50) and 81 (p90), and for FY 2009 were 72.2 (p50) and 81.3 (p90), reflecting p90 0.3% improvement.13 Therefore, these data reflect poor outcomes of patients with T2DM with A1c levels that were not controlled at WBAMC.
Uncontrolled diabetes accrues significant health care costs and adverse diabetic outcomes.10 Consequently, the WBAMC clinical operations division, which was tasked to monitor the HEDIS database, identified and contacted individuals to schedule health care appointments. The primary endeavor was an attempt to substantially increase benchmarks and maintain levels of A1c < 9%, demonstrate improvement in quality of care, and reduce health care costs. Unfortunately, these goals were not met for the aggregate of patients with T2DM.
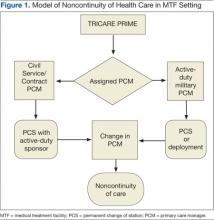
Figure 1 illustrates how the diabetic population at WBAMC had experienced decreased continuity of care and the adverse effects on their diabetes management. Figure 1 also illustrates how beneficiaries of TRICARE are assigned a PCM and how this process results in a lack of continuity of care for patients with T2DM. An Army medical center (MEDCEN) typically uses PCMs who may be a physician, nurse practitioner (NP), or physician assistant. Unfortunately, the majority of these PCMs are active-duty military or civil service personnel who commonly undergo permanent change of station moves or deployments every 3 years. Additionally, military providers are often rotated through department-chief positions, thereby dissolving their patient relationships.