Elder abuse represents a mounting and alarming national health problem that is likely to continue to grow as the older adult population in the U.S. increases from 35 to 72 million by 2030.1 Elder abuse was first described in the 1970s with colloquialisms such as “granny battering” or “elder mistreatment.”2
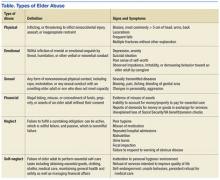
The National Research Council defines elder abuse as “intentional actions that cause harm or a serious risk of harm to an older adult by a caregiver or other person who stands in a trust relationship to the elder, or failure by a caregiver to satisfy the elders’ basic needs or to protect the elder from harm.”3 Elder abuse can further be differentiated into 6 types of abuse: physical, emotional, sexual, financial, neglect, and self-neglect (Table).
According to a National Research Council panel, an estimated 1 to 2 million Americans aged ≥ 65 years have been injured, exploited, or otherwise mistreated by someone on whom they depend on for care or protection.4 For each reported case of elder abuse, 5 more cases go unreported.5 Neglect is the most common type of abuse, followed closely by financial exploitation. Studies suggest that those aged > 80 years are 2 to 3 times more at risk for being abused compared with individuals aged between 65 and 80 years.5 Ninety percent of elder abuse occurs at the hands of perpetrators known to the victim, including 33% by adult children, 22% by other family members, and 11% by spouses or intimate partners.5 More than half, or 53%, of alleged perpetrators of elder abuse are female, and older women are 2 times more likely than men to be abused.6 Nevertheless, it should be noted that one-third of all cases of abuse occur to men, which contradicts myths that they are seldom at risk.
Recent data show that elder abuse also is detrimental to social, law, and health systems.7 Victims of elder abuse have decreased access to support systems and fewer physical, psychological, and economic reserves.7 As a result, the impact of a single incidence of elder abuse is magnified: Victims have a higher 10-year mortality and morbidity than that of older adults who have not been abused, they have significantly higher emergency department (ED) utilization and higher hospitalization rates, and they face an increased risk for institutionalization.7,8 Economic estimates suggest that cases of elder abuse contribute to more than $5.3 billion to the annual health care expenditure in the U.S.9
On the micro level, a busy clinician who sees between 20 to 40 patients daily could encounter at least 1 victim of elder abuse per day.10 Nevertheless, a national Adult Protective Services (APS) survey recently suggested that health care professionals (HCPs) were responsible for submitting 11.1% of all elder abuse reports—with physicians accounting for only 1% of reported cases.7 Several factors may help explain the reasons that so few physicians report elder abuse, including a lack of sufficient knowledge on elder abuse definitions, types, risk factors, signs and symptoms; a misunderstanding of the reporting process; or an unwillingness to get involved. A 2005 survey of almost 400 family and internal medicine physicians showed that 63% had never asked their patients about elder abuse, 98% said there should be more education on elder abuse, and 80% felt they had not been trained to diagnose elder abuse.11
Elder Abuse Legislation
The Elder Justice Act was enacted as part of the Patient Protection and Affordable Care Act in March 2010 and marked the first piece of federal legislation passed to authorize federal funds to address elder abuse, neglect, and exploitation. An Elder Justice Coordinating Counsel and an advisory board were established as national leadership in the HHS. Under this leadership and support of HHS Assistant Secretary for Aging Kathy Greenlee, an Elder Justice Interagency Working Group (EJWG) was formed in 2012 to further explore the national problem of elder abuse, neglect, and exploitation. The EJWG developed an elder abuse roadmap to provide a detailed, practical guide for teams, communities, states, and national entities, fostering a coordinated approach to reduce elder abuse, neglect, and exploitation.12
The roadmap includes initiatives such as the development of an interactive, online curriculum for legal aid and civil attorneys to identify and respond to elder abuse, what lawyers need to know about elder abuse by the Department of Justice, and the development of a voluntary national APS data system to collect national data on elder abuse by the HHS. Also there has been private stakeholder action by the Archstone Foundation/Keck School of Medicine of the University of Southern California, which is developing a national training initiative, and the Harry and Jeannette Weinberg Center for Elder Abuse Prevention at the Hebrew Home at Riverdale in New York, which is working on the development of emergency shelters for elder abuse victims.12 The 2015 White House Conference on Aging also has made elder justice one of its 4 tracks that aims to support the “dignity, independence, and quality of life of older Americans at a time when we’re seeing a huge surge in the number of older adults.”13